
Craniomandibular Dysfunction
Craniomandibular Dysfunction
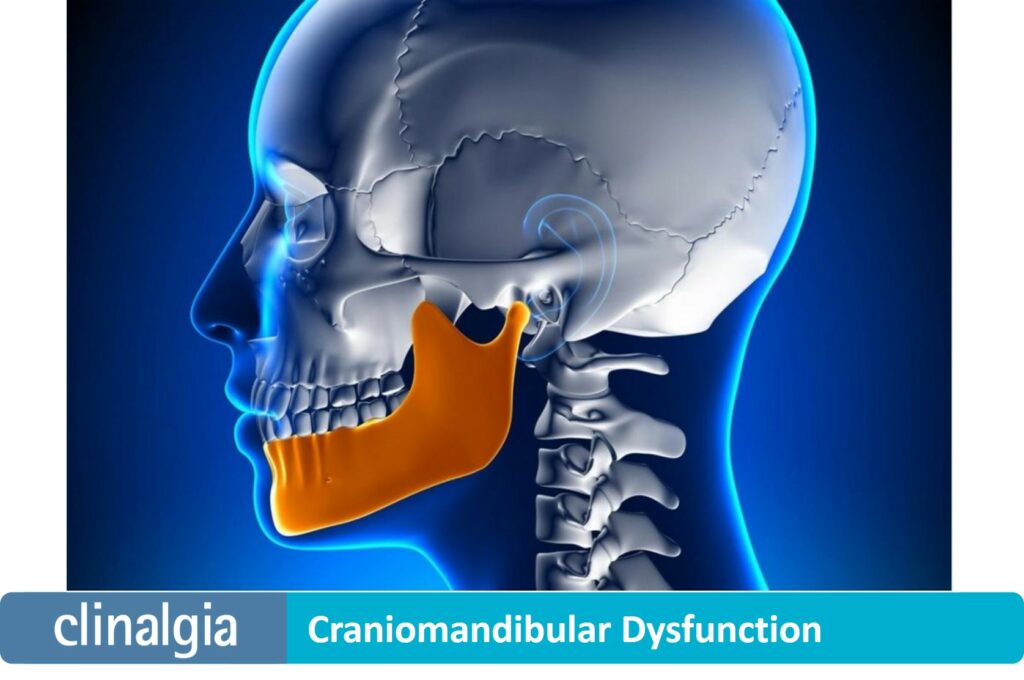
Craniomandibular dysfunction (CMD) or temporomandibular dysfunction (TMD) refers to problems related to the jaw, related muscles, ligaments and tendons.
Typically, patients suffer from pain and/or limitation of jaw mobility, which often affects chewing.1
It is the most common orofacial pain, after pain due to tooth decay or gum and supporting bone (periodontal) disease.2
Symptoms of craniomandibular dysfunction
Initially, any disease causing the symptoms should also be ruled out and the patient should be referred to an expert, usually a dentist or maxillofacial surgeon.
Since the jaw muscles extend to the surface of the skull and the cervical region, these patients often also suffer from headaches and neck pain.3
Sometimes the way the upper and lower teeth relate to each other (occlusion) makes chewing function difficult and overloads the jaw muscles and joints.
Treatment of temporomandibular dysfunction
The use of occlusion stabilizing splints, occlusal adjustments, physiotherapy or muscle infiltration is important in these cases.
Years ago it was understood that establishing a certain meshing between the upper and lower teeth was fundamental, which led to extensive, invasive and costly dental treatments that could even worsen the case.
Today this is not justified, and experts agree on the importance of being cautious and avoiding irreversible treatments, such as orthodontics or restoration with dentures.4
If temporomandibular dysfunction is not resolved, over time it can become a pain that spreads to other regions of the body (head, neck, chest, back…) or even affect the patient emotionally.
There is increasing evidence that craniomandibular dysfunction pain shares central sensitization mechanisms with fibromyalgia, irritable bowel syndrome or chronic fatigue syndrome.5
References:
-
-
- Gauer RL, Semidey MJ. Diagnosis and treatment of temporomandibular disorders. Am Fam Physician.2015; 91:378-386.
- Jerolimov V. Temporomandibular disorders and orofacial pain. Rad 504 Medical sciences 2009; 33:53-77) (Šklebar D, Šklebar I, Cesarik M, Barada A, Maletić A. Neuropathic orofacial pain – diagnostic and therapeutic challenges. Period Biol. 2015; 117:231-237.
- Gonçalves DA, Camparis CM, Speciali JG, Franco AL, Castanharo SM, Bigal ME. Temporomandibular disorders are differentially associated with headache diagnoses: a controlled study. Clin J Pain. 2011; 27:611-5.
- Greene CS. The etiology of temporomandibular disorders: implications for treatment. J Orofac2001; 15: 93-105.
- La Touche R, Paris–Alemany A, Hidalgo-Pérez A, López-de-Uralde-Villanueva I, Angulo-Diaz-Parreño S, Muñoz-García D. Evidence for Central Sensitization in Patients with Temporomandibular Disorders: A Systematic Review and Meta-analysis of Observational Studies. Pain Pract.2018; 18: 388-409.
-


