
Myofascial Pain Syndrome
Myofascial pain syndrome comes from the word «mio» which means «muscle» and the word «fascia» which refers to a system of connective, elastic tissue that envelops the structures that make up our body.
-
-
- What is myofascial pain syndrome?
- How is it generated?
- Symptoms
- Prevalence
- Cellular biology
- Importance of chronic pain syndromes
- Treatment
-
1.- What is Myofascial Pain or Myofascial Pain Syndrome?
The fascial system connects all our organs, since it extends uninterruptedly from the surface of the entire muscular system (under the skin) to the membranes of our cells, including all the envelopes of our organs, blood vessels, nerves, etc.
When we speak of myofascial pain, we are referring to pain that is triggered in relation to certain tense bands that are formed by repeated muscular over-activation.
The muscles and their fasciae are shortening, tractioning and compressing structures, which produces pain and other sensations.
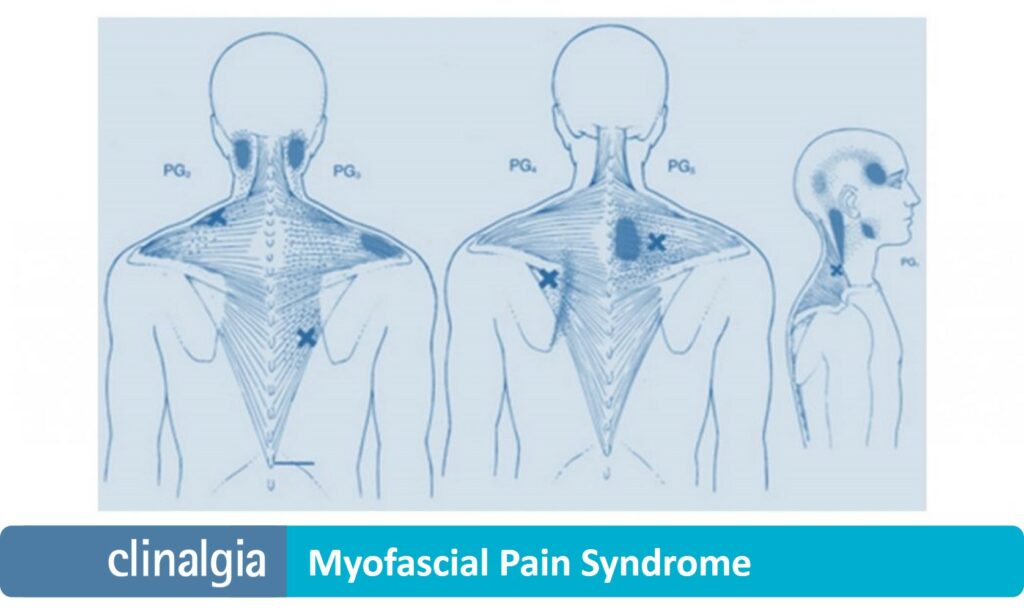
Trigger points, so called because they «trigger pain» that typically radiates to other areas of the body, are usually explored on these tense bands.
2.- How is it generated?
When muscles work, there is a shortening of the fibers that constitute them, giving rise to an approximation between their ends that we call muscular contraction.
The work of a muscle is the result of the work of all the muscle fibers that compose it, and which are united under the same envelope (fascia).
The genesis of myofascial syndromes has been related to muscle overuse or overload, which perpetuates the activation of the muscle fibers, which become exhausted and fibrotic.
Fibrosis leads to loss of elasticity, contractile capacity and oxygenation of the muscles. Tight bands and «knots» of contraction that we can explore on our muscles are thus formed.
The origin of muscular over-activation is diverse. In general, it is related to repeated mechanical efforts, poor postural hygiene and/or emotional stress.
3.- Symptoms of myofascial pain syndrome
The main symptom of myofascial pain syndrome is pain related to trigger points and tight bands. This pain is manifested or increased by pressing on the shortened muscle structures.
It is characteristic that when stimulating these areas the patient perceives pain at a distance, in areas that theoretically do not relate to those where the trigger points are located.
For example, a trigger point in the temporalis muscle may radiate to a tooth with pulpitis characteristics, a trigger point in the muscles of the nape of the neck (suboccipital) may «trigger» a migraine, and trigger points in the quadratus lumborum may well mimic the pain of nephritic colic.
In addition to pain, in myofascial syndromes there is also loss of strength and lack of muscle coordination, postural changes, arthritis or dysesthetic sensations (numbness, tingling, burning or electrical sensations, etc).
This is why myofascial syndrome can be considered as «the great faker», which can distort painful sensations and manifest itself on healthy structures, confusing the physician and the patient.
Prevalence
It can be considered the most frequent pain of mankind, although it is perhaps the least diagnosed, since it cannot be objectified with any usual diagnostic test. It must be explored.
We must consider that our musculo-fascial system is the one that is most activated in stressful situations, whether it is a mechanical or emotional stress.
It is very important to approach the myofascial syndrome in any other chronic painful process, regardless of its nature and location.
The explanation is the «alert and immobilized state» with which our muscles react to any other local pain.
For example, only by ruling out myofascial pain in the musculature related to a painful hip will we be able to assess how much the joint really hurts.
Our protocols organize a previous myofascial treatment, which once controlled allows us to decipher other painful structures to be treated in a more specific way and with a higher probability of success.
5.- Cellular biology
When the areas of tight bands and trigger points are studied in depth, the following phenomena are observed:
-
-
- Maintained excitability of muscle cells. They are recorded with microscopic electromyography. This phenomenon can sensitize neurons of the pain regulatory system (nociceptive), causing radiating (referred) pain and other symptoms.
- Inflammatory molecules. These also stimulate the nociceptive system and/or produce local inflammation that may end up overstimulating other neurons of the central nervous system.
- Ischemia. It is the lack of oxygenation, possibly caused by the lack of mobility of the affected areas.
-
Importance in chronic pain syndromes.
Chronic pain favors muscle shortening maintained as a logical reaction in order to immobilize and protect the damaged area (protective contraction).
The myofascial component needs to be thoroughly explored in all patients with chronic pain.
Chronic pain often encompasses several components, which need to be explored and addressed separately.
Treating the myofascial component of pain will promote a beneficial response if we subsequently treat arthritic or neuropathic pain.
Myofascial pain has to be considered in patients with neck pain, low back pain, craniomandibular pain, chronic widespread pain with central sensitization, fibromyalgia, etc.
It can even be limiting in patients with oncological pain, especially around areas treated with radiotherapy.
7.- Treatment of Myofascial Pain Syndrome
Pain in myofascial syndrome responds poorly to medication. It will be necessary to work the tense bands and myofascial retractions with different strategies.
There are very specific physiotherapy techniques, and the efficacy of infiltrations and dry needling for the dissolution of muscle shortening and recovery of myofascial elasticity has also been described.
Our protocols apply very superficial local anesthetic, medical ozone and specialized physiotherapy techniques.
We manage to deprogram the musculature, reoxygenate the tissues and recover their mobility and elasticity (optimization of muscular and myofascial chains).
It is also important, from the Bio-Psycho-Social point of view of pain, to educate the patient to understand their problem and work on their biomechanics, as well as to avoid triggers, such as overexertion, poor posture, sleep problems or psychological problems.