Trigeminal Neuralgia
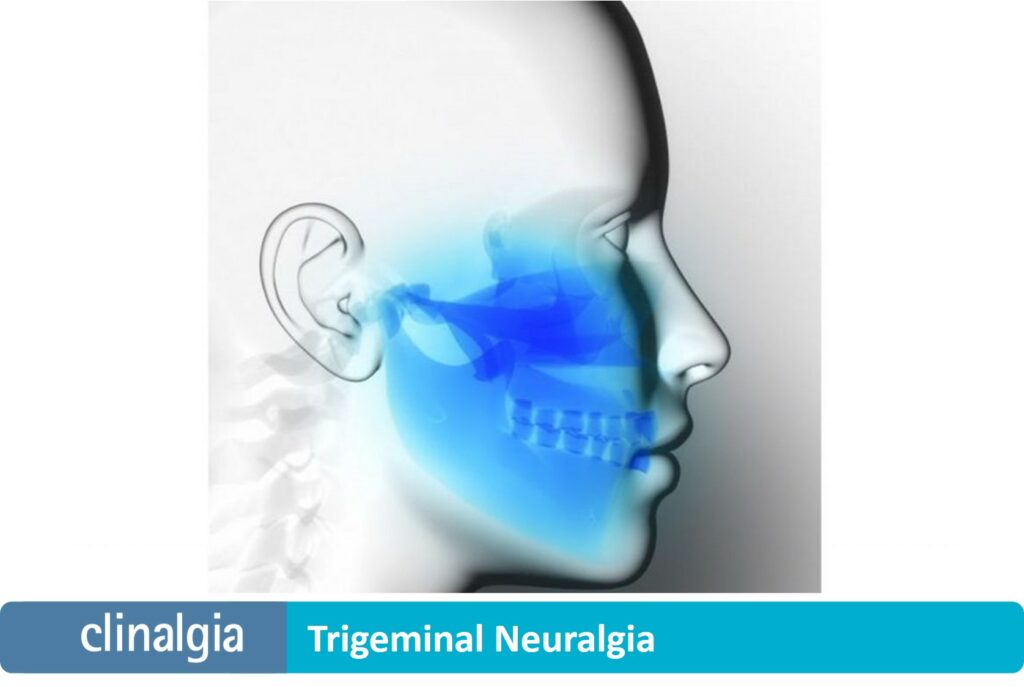
Pain related to the trigeminal nerve is usually unilateral, in the form of crises, corresponding to one or more of the three branches of the nerve.
What is trigeminal neuralgia?
Trigeminal neuralgia is a type of chronic pain affecting the face. It causes pain, sudden burning or a feeling of extreme shock.
The first branch would affect the upper part of the face (around the eyebrow), the second would affect the middle third (around the nose and upper lip), and the third would affect the lower third (lower lip area).
The crises are strictly confined to these areas and involve outbreaks of very severe, incapacitating, immobilizing pain, which prevents any activity.
The pain is usually defined as «ramps», or «electric shocks», which generally last seconds and are triggered by the slightest stimulus: rubbing against the skin, blinking, chewing or swallowing (1).
These painful crises can occur isolated in time, or follow one after the other, continuously, without allowing the patient to relax, generating fear and anxiety.
Types of neuralgia
Trigeminal neuralgia was first mentioned in a medieval Persian text, shortly after the year 1000, although it was not described in the medical literature until 1677 (2).
Its cause was unknown for years, although already in this writing the possibility of a blood vessel irritating the nerve root by compression is referred to, a hypothesis that was not proven until the recent 1970s (3).
Currently, three types of trigeminal neuralgia can be classified:
-
-
- Classic neuralgia: morphological changes in the nerve root are evidenced, due to compression of the nerve root by a blood vessel.
- Secondary neuralgia: caused by a specific disease, such as multiple sclerosis or a tumor, especially meningiomas or posterior fossa neuromas.
- Idiopathic. There is no known cause.
-
Pharmaceutical treatments
The treatment of choice is the administration of carbamazepine or oxcarbazepine, the antiepileptic drugs with the highest level of evidence.
These drugs require periodic blood tests to assess hepatic and renal function (4).
Systemic ozone therapy, perfectly tolerated, has demonstrated its protective efficacy in these organs, and can be an alternative in delicate patients who need this medication to have quality of life (5-12).
If vascular compression is detected, treatment with microsurgery to free the nerve root will be considered (13).
In cases in which the neuralgia does not respond to carbamazepine or oxcarbazepine, other medications can be tried, generally central nervous system depressants, since the aim is to reduce the excitability of the trigeminal neurons.
Baclofen or lamotrigine, among others, could be tried (14).
If a single drug is not effective, a combination of several drugs may be used.
In any case, doses and medications should be adjusted sequentially, according to the efficacy and tolerability of each patient.
Alternative treatments
If there is no improvement with pharmacological treatments, we would move on to invasive treatments, firstly by carrying out small peripheral blocks on the «trigger» areas (whose stimulus «triggers» the crises).
These can be repeated periodically, as they are hardly bothersome and the risk is minimal. This strategy has been shown to enhance the effect of medication (15).
An alternative for the most stubborn cases would be percutaneous rhizotomy.
This involves selective injury (thermal, chemical or compressive) to the affected trigeminal ganglion or roots.
Not without complications, this technique has shown favourable results, always in expert hands (16).
References:
-
- Harris W. Chronic paroxysmal trigeminal neuralgia. Neuritis and neuralgia. Oxford: Oxford University Press 1926; pp.150–222) (Kugelberg E and Lindblom U. The mechanism of the pain in trigeminal neuralgia. J Neurol Neurosurg Psychiatry 1959; 22: 36–43.
- Dewhurst K. A symposium on trigeminal neuralgia. J History of Medicine 1957; 12: 21–36.
- Jannetta PJ. Observations on the etiology of trigeminal neuralgia, hemifacial spasm, acoustic nerve dysfunction and glossopharyngeal neuralgia. Definitive microsurgical treatment and results in 117 patients. Neurochirurgia (Stuttg) 1977; 20: 145–154.
- Al-Quliti KW. Update on neuropathic pain treatment for trigeminal neuralgia. The pharmacological and surgical options. Neurosciences (Riyadh) 2015; 20: 107-114.
- Peralta C, Xaus C, Bartrons R, León OS, Gelpi E, Roselló-Catafau J. Effect of ozone treatment on reactive oxygen species and adenosine production during hepatic ischemia-reperfusion. Free Rad Res 2000; 33:595-605.
- Candelario-Jalil E, Mohammed-Al-Dalain S, Fernández OS, Menéndez S, Pérez-Davison G, Merino N, Sam S, Ajamieh HH. Oxidative preconditioning affords protection against carbon tetrachloride-induced glycogen depletion and oxidative stress in rats. J Appl Toxicol.2001; 21:297-301.
- Ajamieh H, Merino N, Candelario-Jalil E, Menéndez S, Martinez-Sanchez G, Re L, Giuliani A, Leon OS. Similar protective effect of ischaemic and ozone oxidative preconditionings in liver ischaemia/reperfusion injury. Pharmacol Res.2002; 45:333-339.
- Ajamieh HH, Menéndez S, Martínez-Sánchez G, Candelario-Jalil E, Re L, Giuliani A, Fernández OS. Effects of ozone oxidative preconditioning on nitric oxide generation and cellular redox balance in a rat model of hepatic ischaemia-reperfusion. Liver Int.2004; 24:55-62.
- Ajamieh HH, Berlanga J, Merino N, Sánchez GM, Carmona AM, Cepero SM, Giuliani A, Re L, León OS. Role of protein synthesis in the protection conferred by ozone-oxidative-preconditioning in hepatic ischaemia/reperfusion. Transpl Int.2005; 18:604-612.
- León OS, Ajamieh HH, Berlanga J, Menéndez S, Viebahn-Hánsler R, Re L, Carmona AM. Ozone oxidative preconditioning is mediated by A1 adenosine receptors in a rat model of liver ischemia/ reperfusion. January 2008; 21:39–48.
- Gultekin FA, Cakmak GK, Turkcu UO, Yurdakan G, Demir FE, Comert M. Effects of ozone oxidative preconditioning on liver regeneration after partial hepatectomy in rats. J Invest Surg.2013; 26:242-252.
- Aslaner A, Çakır T, Çelik B, Doğan U, Akyüz C, Baştürk A, Polat C, Gündüz U, Mayir B, Şehirli The protective effect of intraperitoneal medical ozone preconditioning and treatment on hepatotoxicity induced by methotrexate. Int J Clin Exp Med. 2015; 8: 13303–13309.
- Cruccu G, Gronseth G, Alksne J, Argoff C, Brainin M, Burchiel K, Nurmikko T, Zakrzewska JM; American Academy of Neurology Society; European Federation of Neurological Society. AAN-EFNS guidelines on trigeminal neuralgia management. Eur J Neurol.2008; 15:1013-1028.
- Lunardi G, Leandri M, Albano C, Cultrera S, Fracassi M, Rubino V, Favale E. Clinical effectiveness of lamotrigine and plasma levels in essential and symptomatic trigeminal neuralgia. 1997; 48:1714-1717.
- Lemos L, Fontes R, Flores S, Oliveira P, Almeida A. Effectiveness of the association between carbamazepine and peripheral analgesic block with ropivacaine for the treatment of trigeminal neuralgia. J Pain Res.2010; 3:201-212.
- Pollock BE. Surgical management of medically refractory trigeminal neuralgia. Curr Neurol Neurosci Rep.2012; 12:125-131.